Gary Sheehan joined us on the CoffeeTalk: COVID-19 Business Impact to give his perspective.
Transcript of the above discussion
Q: Can you tell us a little bit about your business model and how it’s changed with COVID-19?
Gary: Cape Medical Supply is based in Massachusetts, operating in Massachusetts, Rhode Island, New Hampshire and Maine. We’re a sleep company with an orthopedic bracing line of business, but about 85 percent of our revenues derive from sleep therapy products and services.
Like most Americans, I watched COVID-19 unfold through January as just a citizen and then in late February, I began to watch it more as an HME provider with a growing sense of concern about what the impact was going to be here in the United States and how we would react as an organization.
The week of March 9, we began to plan and went “far and fast”. By March 13, we moved all of our employees home and, effective March 16, discontinued all patient contact. That same day, we began contact with payer partners. They were very supportive of our plans and ability to continue to service beneficiaries remotely.
Now, we’ve got four people in our warehouse manning our pick, pack, ship operation and one to two clinicians a day setting and shipping devices for new CPAP and BiPAP patients. We built out an extensive video library to support the initial adherence and compliance. And we have both our clinicians and customer support teams working from home reacting within their call queues.
We’ve learned a lot through the first several weeks of this but the business is functioning largely as normal. It’s been a credit to our management team and all of our employees. They’ve embraced this challenge and are continuing to deliver a high level of patient care across the four states. The support from payers and referral partners has been fantastic.
Q: What are you doing differently to support your patients and your referral sources?
Gary: First in our mind was to ensure the health and safety of our team members. A very close second to that was the continuing service of both our patients and referral partners. It’s really about leveraging technology, both telephonic and video technology, to support our patient base and make sure that they have the resources that they needed.
We’ve got a pretty large group of clinicians that were previously out across four states meeting face-to-face. Now, they’re in their homes and available for telephonic consults with the patients, and helping them orient to therapy.
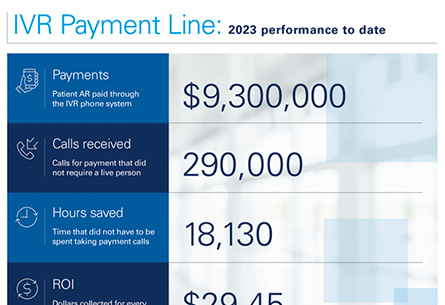
Regarding referral partners, this shift was not a result of a heroic weekend of work. This was years of investment in technology, partnering with companies like Brightree and having our phone system ready to go. Our people took the phones off their desks, plugged them in at home and were right away in their same call queues. We had an infrastructure in place that was ready to react to a situation like this.
That first week, there was a lot of learning for our team. The second week, I wrote a playbook for referral partners to help them operate in a telehealth environment. Many of our referral partners are small businesses themselves and they’re struggling for how they’re going to survive and take care of their patients in this environment too. We’d done a lot of research and legwork to build our plans and are closely following guidance from CMS and commercial payers in New England, so we felt like we had some knowledge we could impart. The playbook covered how to leverage telehealth and home sleep testing in this new world – and our sales team began sharing it widely across the region, where it’s been well received by our referral partners.
Q: How are you getting products to patients?
Gary: Shipping. We have our own pick, pack, ship facility and we also partner with VGM for redundancy. In March, that facility had one of its busiest months ever. Patients are very focused on hygiene and cleanliness in this sort of environment.
We were able to shift things around and build out a new supply shipments center within the facility to allow our clinicians, state licenses respiratory therapists, to work with the devices and set them to the physician’s requirements as dictated on the prescription. We just added that as a component of the facility and it meets all of the physical distancing recommendations that have come from the Massachusetts governor and the federal government.
Q: Are you set up to handle potential COVID-19 discharges or having COVID-19 patients in your care? Have you thought through that process?
Gary: We’re paying attention to that on a few fronts. For returned packages, we’ve implemented a segregated receiving area where we’re not touching any packages that come in for three business days.
In terms of newly diagnosed patients, we’re closely following the evolving medical science and focusing on where BiPAP therapy is going to fall in the treatment protocol. We feel we can use our existing workflows and pathways to deliver path devices to newly diagnosed patients or suspected diagnosed patients.
We are in early discussions with partners about a potential hospital diversion plan that would involve BiPAP therapy in the home, but we would do that remotely, the same way that we’ve done shipments to date. We’ve learned a lot about the right digital resources to pair with shipments and are going to apply that learning to any positive patients that come our way.
Q: Are you experiencing any equipment shortages in concentrators or PPE for your employees?
Gary: PPE shortages are very real, but because we’re not seeing patients, it’s not as critical of a need for us right now. We are working with the New England Association to potentially handle a bulk order of PPE that we can then distribute to HME providers across New England. Our bracing business is a consignment model; those are primarily distributed through hospital emergency departments and urgent care centers.
We’re continuously supplying our technician there with PPE and but the situation in these hospitals is very fluid. There’s a few of them that aren’t even allowing us in anymore; we’re just delivering and they’re stocking.
We are aware of significant shortages of concentrators and ventilation devices and are doing anything we can do to support that effort.
Q: Are you still seeing your bracing products prescribed with everything that’s going on with the hospitals?
Gary: Yes, to a much lesser degree. Normal life does not stop. People still break bones, and sprain and get in car accidents and require products and services that come through those programs but people are avoiding emergency departments at all costs, for obvious reasons. I think people are still getting injured but they’re just taking care of themselves, using what they have at home to self-treat with rest, ice, compression and elevation. So the business is off quite a bit there, but we still have to keep things stocked.
Q: What has been your biggest surprise from COVID-19?
Gary: The biggest surprise from a Cape Medical perspective was how seamlessly we have transitioned to this work from home environment. We’re housed in a 15,000 square foot, two-floor building, and there are two people there now. We have these calls that we tick through issues and walk through how the technology is functioning, how the call centers are working… and if you were a long-standing patient of ours and not aware of the COVID-19 situation, you would see no change in how we’re serving you. The resilience of our team members through this process and our ability to conduct business as usual when our entire workforce is in their homes has been the biggest present.
I think that this whole thing is going to change how work is done in America for generations to come. We’re already evaluating what we’re going to do when things go back to “normal.” Questions like: is there a need for everybody to drive into work five days a week? We’ve learned a lot about what we can do remotely, what our capabilities are in this sort of environment, and how great our people are that they can plug in at home and continue the service our patients and partners.